Introduction
Epidermoid or squamous cell cancer of the head and neck (SCCHN) is often a tragic and debilitating disease that is preventable in most cases. As in most cancers, early detection and treatment are the keys to curing these malignant tumors. The strong relationship between these tumors and tobacco and alcohol use is undeniable. Therefore, eliminating such habits goes a long way toward prevention of these cancers. In the last two decades, treatment has focused on ways to cure SCCHN without the functional and cosmetic consequences of radical surgery.
Epidemiology and Risk Factors
Head and neck cancers are seen more often in urban areas in industrialized nations. It is in these areas where tobacco and alcohol use, as well as air pollution, tend to be highest. Tobacco acts directly as a cancer-causing agent and also facilitates the cancerous effects of alcohol. Cigarette smoking can affect the tissues of the entire nose, throat, windpipe (trachea) and voice box (larynx). Marijuana smoke is felt to contain even more cancer-causing agents than tobacco. Chewing tobacco and snuff are most likely to affect the mouth, where they bath the tissues. SCCHN is more common in men and has some hereditary tendency. Other risk factors include chewing Betel nuts and smoking “chutta” (lit end of the cigarette in the mouth), as practiced in some parts of Asia. In China and other Southeast Asian countries one form of SCCHN that begins in the back of the nose (nasopharynx) appears to be related to dietary nitrites contained in smoked fish. This particular tumor has also been linked to the Epstein Barr Virus (EBV). Patients infected with HIV or the AIDS virus are at higher risk of developing SCCHN. In the United States, the frequency of head and neck cancers has been declining as the use of tobacco has become less common.
Presentation and Natural History
Damage to the mucous membranes of the nose and throat from tobacco and alcohol leads to abnormalities in the cells of these tissues. At first there is inflammation and a tendency for the cells to multiply and produce protective materials known as “keratin.” Early on there may be white, raised areas on the mucous membranes known as “leukoplakia.” These contain cancer in less than 1 percent of cases. However, as the tissue damage continues, the areas become red and are referred to as “erythroplasia.” Here the chance of cancerous cells being present is greater than 75 percent.
Head and neck cancer starts in the mucus membranes of the mouth, throat, nose, sinuses, esophagus, trachea, or larynx (see figure below).
Symptoms depend upon where the tumor begins. Hoarseness indicates involvement of the vocal cords. Sore throat can occur from involvement of the tonsils, tongue or other parts of the throat. Nasal blockage with bleeding or swelling of the face may indicate tumor in the nose or sinuses. Sometimes the cancer can be seen as a lump or ulcer in the mouth or nose. Occasionally, involvement of certain nerves can cause symptoms such as weakness of the face, tongue, voice, and swallowing mechanism. The cancer irritating a nerve ending deep in the throat occasionally causes ear pain in the absence of ear infection. Some tumors can grow large enough to block the upper airway, causing noisy, difficult breathing that can become life threatening.
Early cancer of the tongue
Head and neck cancers tend to spread through tiny channels called lymphatics that lead to the lymph nodes in the neck. The lymph nodes become enlarged as they then try to contain and destroy the tumor cells using cells from the immune system. This results in painless, nontender lumps in the neck that grow larger over time. The figure on the left depicts typical patterns of spread into various lymph node groups in the neck by cancers originating in specific areas of the nose and throat. Spread to the neck indicates an advanced stage of the cancer. However, aggressive treatment can still result in a cure.
Although the cancers tend to reveal themselves in the head and neck, there are occasional instances when the tumor has spread (or metasta-sized) to other organs, such as the lungs, bone, brain, and liver. This is usually a late, advanced stage of the cancer that is rarely curable.
Evaluation
Assessing someone with a suspected SCCHN involves a thorough examination of the head and neck by an otolaryngology or head and neck specialist. This involves looking at and feeling the tumor where it begins in the nose, mouth, larynx, trachea or esophagus, as well as any swelling in the neck. A suspicious area can be an ulcer or a red, raised, irregular lump in the mucous membranes. In the neck, swelling can be firm to hard, movable or stuck to the deep tissues, and two to several centimeters in size.
If the cancer is easily accessible (such as the lip or tongue) a simple biopsy can be done with local anesthesia in the office. In this case Novocain is injected into the tissue to numb it, and a small piece of the suspicious area is removed and sent for microscopic analysis by a pathologist. Any lymph node swelling can be assessed by sampling it with a fine needle, sending the aspirated tissue for pathology examination. However, no cuts or open biopsies should be performed on the lymph nodes to prevent spreading the tumor into the surrounding skin and soft tissues.
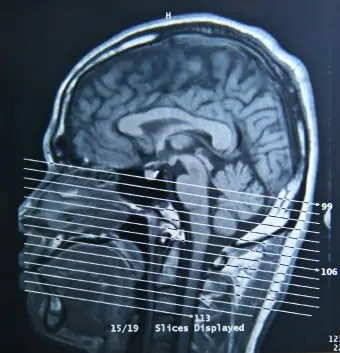
Imaging studies can be useful to show the internal extent of deep tumors and the presence of abnormal lymph nodes that may be difficult to detect. CT (computed tomography) and MRI scans give the most detailed information. More recently, PET (Positron Emission Tomography) scans employ nuclear medicine and digital technology to detect early recurrent cancer or metastases to other organs. The PET scan is particularly useful in following patients after therapy.
All patients with SCCHN should be examined under anesthesia. The “panendoscopy” involves checking the mucus membranes of the nose, mouth, throat, larynx, esophagus, trachea and lung. The purpose is not only to examine deep tumors and obtain biopsies, but also to look for second cancers. Since the tissues of the upper airway and digestive tracts are all simultaneously affected by years of tobacco and/or alcohol exposure, it is not unusual to find two or more cancers in different sites.
Treatment
“Precancers” that exist as leukoplakia or erythroplasia can be treated with Beta Carotene or Vitamin A. There is considerable evidence that these derivatives are protective in patients that may progress toward frank cancer. Beta Carotene is preferred since it is best tolerated. Removing leukoplakia or erythroplasia surgically is often necessary when there is suspicion of cancer in the tissue.
The “early” cancers of the head and neck are typically confined to a smaller area and have not spread to the lymph nodes of the neck. Usually, these tumors are treated with either radiation therapy or surgery. Surgery is preferred when there will be little or no loss of function or change in appearance. It avoids the long-term dry mouth caused by radiation’s affect on the salivary glands. Radiation is preferred when surgery will cause cosmetic or functional deformities or when surgery cannot remove lymphatic tissues that might contain cancer cells (such as in the neck). The oral dryness caused by radiation has been less of a problem in recent years because of the use of medications such as amifostene, which protect the salivary tissues. The early cancers can be cured in 75 to 95 percent of cases. “Cure” is defined as disappearance of the cancer for more than five years.
Advanced cancers are typically larger and involve the lymph nodes of the neck. Classically, both radiation and surgery have been required to control these tumors. The side effects of aggressive surgery and radiation can be devastating. Permanent loss of voice, swallowing and speech problems, shoulder pain and weakness, facial and neck deformity and scar, paralysis of cranial nerves, and loss of vision are a few of the dire consequences. In the last few years, research has uncovered ways to treat these advanced cancers with chemotherapy and radiation therapy with similar cure rates to surgery/radiation. In many cases, vital organs such as the larynx and tongue can be spared and radical operations on the neck can be avoided. The response of the cancer to chemotherapy is often an indicator of how likely the tumor can be cured. A complete disappearance of the cancer after one or two chemotherapy treatment sessions (cycles) typically bodes well for the patient. When the cancer responds poorly to two cycles of chemotherapy, it is often necessary to resort to surgery along with radiation therapy. Chemotherapy and radiation do lead to a short-term “mucositis,” a severe inflammatory reaction akin to a severe burn of the mucous membranes of the mouth and throat. Other reactions include nerve damage and temporary weakening of the immune system. Chemotherapy is often given for several days at a time for several sessions. Radiation is given daily or twice a day for five to seven weeks. Chemotherapy can be given before radiation in so-called “induction” therapy or in between shorter courses of radiation in “concomitant” therapy. Whether the advanced cancers are treated with surgery/radiation or chemotherapy/radiation, the cure rates are typically about 50 percent overall. Most relapses occur within the first year after treatment. Some patients who fail chemotherapy/radiation are candidates for surgical treatment or “salvage.”
Research into other therapies continues, as the cure rate for advanced SCCHN is still poor. It has long been felt that the key to controlling cancer lies in the immune system. Antibodies are proteins that the body produces to fight off infections and to destroy cancer cells. “Monoclonal antibodies” have been produced that direct their efforts against a specific type of cancer cell. These antibodies can be linked to radioactive substances that can then be targeted against the cancer cells. There are still many practical stumbling blocks in using this technology today as research continues.
Conclusion
Cancer of the head and neck can be a devastating disease with complicated treatment regimens and loss of vital functions, such as speech and swallowing. Our best weapon against this disease is prevention. The elimination of smoking and other tobacco use would likely prevent over 90% of these tumors. Although chemotherapy with radiation has helped to prevent the loss of vital organs in this disease, improving cure rates for advanced head and neck cancer will likely require further research into how our immune systems respond to cancer cells.
